Dr. Karen Horton has either authored or reviewed and approved this content.
You will be allowed to go home from the hospital a few hours after outpatient surgery, or you may wish to stay overnight based on your procedure and your surgeon’s recommendations. Another adult needs to stay with you for the first night if you go home. You should have a family member or friend nearby for a few days in case you need help with physical activities such as transportation to your first follow up appointment, child care or lifting more than 5 pounds around your home.
If you have had breast surgery, you will have some mild swelling of the breasts and your breasts may feel “full”. You will either have a loose gauze net dressing or an ACE wrap in place, with some soft pads over your incisions. For abdominal surgery or liposuction, you will be wearing a compressive garment when you awake that will fit snugly but comfortably. You will not need to change any dressings immediately after surgery; you will be able to see your results at your first postoperative visit with your surgeon.
Please make sure that you stay well-hydrated for the first few days after surgery. Your urine should be clear and light yellow rather than dark and concentrated, and you should not feel thirsty: these are signs and symptoms of dehydration!
If drains have been placed, you will care for your drains twice daily at home. You should take it easy and relax as much as possible for a few days. However, “bed rest” is not permitted; you should take short walks around your home or bedroom and exercise your calves and lungs by taking deep breaths and coughing.
You will be seen at the office for your first dressing change a few days after surgery. At this visit, we will provide you with a comfortable postsurgical bra or other post-surgical garments that you will wear for up to six weeks. You do not need to specifically purchase any special postoperative equipment unless your surgeon specially instructs you to do so. We recommend you avoid wearing underwire bras for at least 6 weeks after breast surgery.
To pamper yourself during your recovery, we recommend having a friend or family member help you wash your hair in the sink, or visit a salon for a wash and blow dry (and perhaps splurge on a manicure/pedicure or gentle shoulder massage while you are there!).
At your preoperative appointment, you will be given prescriptions for medications to take after surgery. You can take these to any pharmacy and have them filled before surgery so that they are ready for you when you return home. We will go over with you in detail which medications are recommended and how to take them for the best effect. You do not need to bring these medicines with you to the hospital.
After surgery, you will likely need a narcotic medication for at least a few days. Examples are Vicodin (hydrocodone with Tylenol), Percocet (oxycodone with Tylenol), Tylenol #3 (with codeine), or another narcotic alternative. Please let us know which pain medications you have taken in the past that have worked well for you and we will prescribe these preferentially. Likewise, we will avoid pills that you have not had a good experience with (i.e. stomach upset or allergic reaction). Many narcotic medications are associated with some nausea; try to take your pain pills on a full stomach to avoid gastric upset.
Once your healing is underway and your discomfort is less, you can switch from a narcotic to over-the-counter acetaminophen (regular Tylenol). Be sure to not take more than 4 grams of Tylenol (4000 milligrams) in a 24-hour period – this is equivalent to not more than 8 extra-strength tablets (500 mg each) or not more than 12 regular-strength tablets (325 mg each) per day.
It is important to avoid medications containing aspirin (ASA, Excedrin) or an “NSAID” (non-steroidal anti-inflammatory drug such as Motrin, Ibuprofen, Aleve) for two weeks before and after surgery as these medications increase bleeding and bruising associated with surgery. Free flap patients are an exception to this rule, and will be specifically prescribed 325 mg of aspirin for a month after Microsurgery.
If you suffer from migraine headaches, please check with our office before taking prescription migraine medications for two weeks before and after surgery, as some of these are potent “vasoconstrictors” and can interfere with blood flow and wound healing.
A prophylactic antibiotic will be prescribed for when you leave the hospital. You will also be given an intravenous antibiotic immediately before surgery and during the time that you are in the hospital to prevent against infection. Please remind us of any rashes, hives or other allergic reactions you may have had to antibiotics in the past; we will prescribe a different class of antibiotic for you.
You will be prescribed Ativan (lorazepam), an “anxiolytic” that helps to relax you before and after surgery. Ativan also effective in treating or preventing nausea and pain; in fact, it is used commonly in chemotherapy and many of our breast cancer patients are already familiar with this medication. You can take Ativan the night before surgery to help relax you and to assist with sleep, and also the morning of surgery when you are around 30 minutes away from the hospital. Remember that you must remain “NPO” (nothing to eat or drink for at least 8 hours before surgery). Ativan is a small pill that you can take with just a SIP of water to allow it to be swallowed. You will have Ativan available to you in the hospital for overnight stays; just ask your Nurses for this medication.
Pain medication, anesthesia and surgery in general can create constipation. Many patients do not have a bowel movement for 3-5 days after surgery – this is entirely normal, albeit uncomfortable. It is important to drink a lot of fluids for a week or two after surgery to stay well-hydrated and to take an over-the-counter stool softener such a Colace (docusate) each day after surgery at home until you have stopped taking narcotic pain medication or are having regular bowel movements.
If you have not had a bowel movement by postoperative day 5, please notify our office and we will help coach you over the phone! Natural remedies such as pear nectar or prune juice, and over-the-counter laxatives such as Dulcolax, Senokot (senna), milk of magnesia or Miralax are often effective if you require additional help having a bowel movement. For safety and comfort, remember to take just one at a time and give each constipation medication up to 12 hours to take effect before trying another!
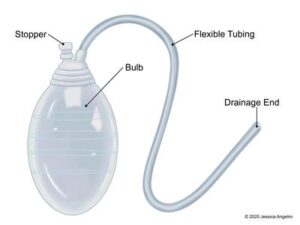
Drains are small, soft silicone tubes that remove blood and wound fluid from around a breast implant or from inside a wound while you heal. There is a small stitch holding the drain in place, and you may have a special dressing over the drain exit site. The drain tubing is attached to a small “JP” bulb that collects wound fluid by way of gentle suction. You will see a drain at your preoperative visit and will be instructed on drain care by our office and again by Nurses in the hospital before you go home. Drains are not used in liposuction procedures.
Drains are not painful, and using drains decreases your risk of complications (infection, capsular contracture, seroma and wound healing difficulties). Use of drains also decreases surgical swelling after surgery, speeding up healing. Please don’t be afraid of drains: they can be a temporary nuisance, but they are important to your healing. In fact, “drains are your friends”!
 We urge you to read Dr. Horton’s blog post on surgical drains and watch all of the accompanying videos so that you are well prepared to care for your drains after surgery.
We urge you to read Dr. Horton’s blog post on surgical drains and watch all of the accompanying videos so that you are well prepared to care for your drains after surgery.
Download our customizable drain log to facilitate easy recording of drain output after your surgery.
The initial drain liquid will be thick, dark or bright red and bloody (“sanguinous”). It will change gradually over a few days to a clear, light yellow (“serous”) wound fluid. You will be given a measuring cup to help record the amount of fluid your drains are producing at the hospital or at our office. Measurement of drain fluid will be in “cc’s” (milliliters, or mL).
You can clip your drains to your bra or your clothing using safety pins after breast surgery, or they may be secured to your abdominal binder by a special Velcro strip after abdominoplasty or an abdominal flap reconstruction. Some women carry their drain bulbs around in a small pouch that hangs around their neck after mastectomy and reconstruction; some breast health centers have these pouches available to breast cancer patients during their recovery.
“Milking” your Drains (stripping the tubes using an alcohol swab) two or three times a day is important to ensure you have a constant flow of wound fluid into the drain bulb and to encourage any clots that form in the drain tubing (this is normal) to travel into the drain collection bulb. If your drain is leaking from around the drain site in the skin, milking the drain will alleviate a fluid build-up and allow better flow into the JP collection bulb. You will be instructed on how to milk your drains before your surgery, at the hospital and again at your follow up visits.
If you have had breast implants placed, you should Remain on Antibiotics and avoid showering until after your drains are removed. You will be given a refill on your antibiotic prescription to fill until your drains are out for breast implant procedures. For all non-implant procedures, you may stop your antibiotics when you finish your prescription, even if you still have drains in place.
You will be Allowed to Shower with your drains only if you have had a tummy tuck or a flap procedure. A practical suggestion for showering with drains is to hang a long ribbon or necklace around your neck and clip the drains using safety pins to the ribbon so that they do not dangle down and create discomfort. This will be described further at your preoperative appointment at our office. Ask us about your specific postoperative instructions if you are unclear about showering.
Please call our office if your drains are producing more than 100 cc a day of thick, red blood. This could be a sign of bleeding and requires evaluation by your surgeon. Please call our office at 415-570-7352 with any questions or concerns about your drains. Our 24-hour answering service will direct your call to your surgeon after-hours.
Drains are Ready for Removal in the office when the color is light and clear yellow and the total fluid output is Less Than 30 cc in a 24-hour Period. Removal of drains does not hurt! The stitch is removed and they are gently pulled out by your surgeon or our nurse.
As long as you have a valid driver’s license (the first requirement!), you can resume driving when your head is clear (not dizzy or drowsy on pain medication or Ativan) and you feel physically and psychologically ready to drive. Many patients feel at ease driving around 2 weeks for most procedures. For breast procedures, some women feel most comfortable with a soft pillow between their chest and the seat belt to avoid direct pressure on their surgical sites.
Returning to work is a judgment call and a personal decision. It is recommended that you take at least a few days off after minor procedures, up to six weeks or more for major surgery or for multiple procedures done at once. This will be discussed with you at your preoperative visit. For reconstructive procedures where medical leave or disability claims are involved, we offer the service of completing the necessary paperwork for you including your return to work details. Nurse Mari will be your contact for return-to-work forms.
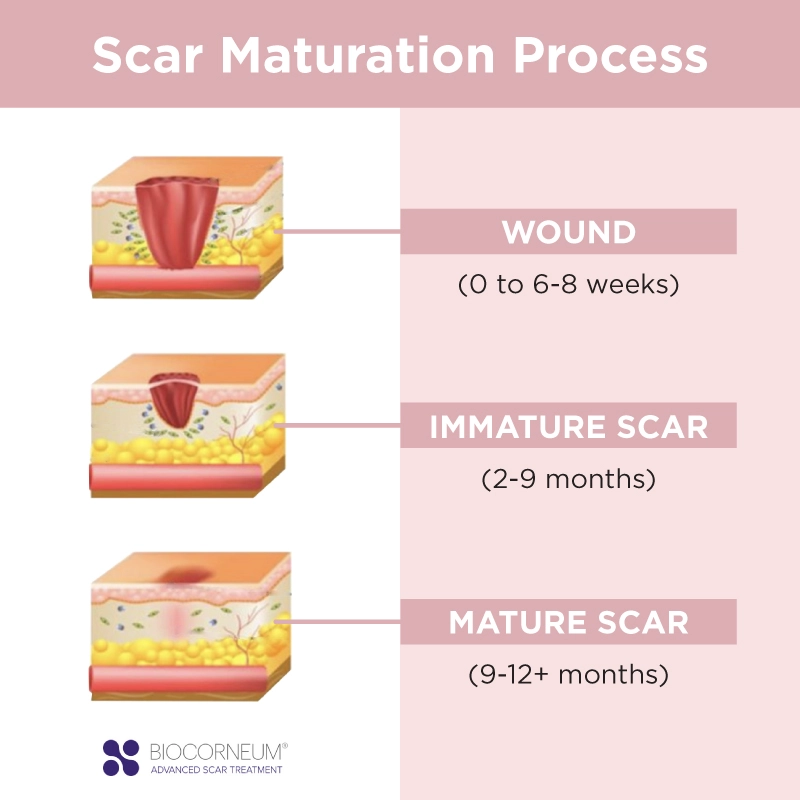 Scar quality is for the most part genetically determined. We look to other scars on your body to see how you naturally heal. Be patient while you are healing and rest assured that time is the most important factor in scar healing. It takes At Least a Full Year for your scars to be fully “Mature”. “Immature” Scars are pink or red, raised, and occasionally can be itchy or tender. In contrast, Mature Scars are flat, soft and supple to the touch and faded, without any symptoms such as itching or discomfort.
Scar quality is for the most part genetically determined. We look to other scars on your body to see how you naturally heal. Be patient while you are healing and rest assured that time is the most important factor in scar healing. It takes At Least a Full Year for your scars to be fully “Mature”. “Immature” Scars are pink or red, raised, and occasionally can be itchy or tender. In contrast, Mature Scars are flat, soft and supple to the touch and faded, without any symptoms such as itching or discomfort.
A Hypertrophic Scar is bright pink or red, is raised, can itch and be painful. Hypertrophic scars can occur most commonly in young people (teenagers) or have a genetic predisposition (run in families). In contrast, Keloid Scars are much more rare and are actually a form of a benign “scar tumor”. Keloid scars grow beyond the original boundaries of the incision and continue to be biologically active even years after the wound has healed. They have many of the same symptoms as hypertrophic scars but are more difficult to treat.
During the first year after surgery, your surgeon will follow up with you regularly and evaluate how you are healing. We recommend “scar therapy” starting at around a month after surgery. During the first four weeks postop, your incisions are still considered “wounds”. You may notice small scabs or weepy areas of healing – this is entirely normal, particularly if a breast reduction or a lift has been done. After a month, scar tissue has formed and the wound healing is well underway; your incisions are then considered to be “scars”.
Scar Therapy consists of Massaging Your Scars and using Topical Scar Gel that contains silicone. Topical silicone together with pressure (via massage or scar strips) is the only therapy that has been clinically proven to speed up scar maturation and improve the appearance of scars. Please ask us about products available for purchase in our office to facilitate scar maturation and softening.
Scar Massage involves applying firm direct pressure on your scars using your fingers by pressing or pinching the scars, together with a silicone-containing scar gel. Beginning at a month postop, you will be taught to massage your scars, particularly at areas of firm swelling. You cannot hurt your incisions, nor can massaging the scars create wound problems. You should avoid areas that are slow to heal or still have scabs attached. You will be instructed on scar massage at your regular follow ups.
It is also extremely important to Avoid Direct Sun Exposure on your incisions for the first year after surgery. Applying Sunblock of at Least SPF 30 to your incisions and any areas of redness or bruising is recommended while you are healing under light clothing and even under a swim suit if you will have sun exposure. Healing scars are prone to “hyperpigmentation”, which is semi-permanent darkening of the scars that can persist over years, particularly in those with dark complexions.
If scars are showing a propensity to become hypertrophic or develop features of a keloid, then additional treatments may be recommended. After routine scar therapy, Steroid Injection of a medication called Kenalog (triamcinolone) mixed with local anesthetic may be administered by your surgeon at an office visit. Up to three injections at 6 week intervals can help alleviate itching and pain for these types of scars.
Surgical Revision is usually the final treatment for scars that are raised, symptomatic, or stretched. Scar revision can be done in the office for small areas or occasionally in the operating room if combined with other procedures. Occasionally steroid is injected at the time of wound closure for especially problematic scars. Scar revision is not usually recommended until 6-12 months have passed, to give your body time to heal first.
Following a breast augmentation, breast lift, breast reduction or reconstruction, you should avoid lifting more than around 5 pounds for approximately 2 to 3 weeks after surgery (this includes heavy laptops, handbags, and children and pets!). Avoid activities that raise your heart rate and blood pressure for the first few weeks after surgery such as exercise or excessive straining, as these may create undue swelling and discomfort. Take it easy and allow your body to heal uneventfully.
At a month postop (up to six weeks for flap reconstructions), you may resume exercise as your body feels comfortable. “Listen to your body” is our mantra for post-surgical physical activities. Your body will tell you when it is ready to resume exercise, and how quickly to increase your efforts. If you are still sore, accept this as a sign that you are still healing and take it easy for a few more weeks.
If you are over the age of 40 years, you should have a baseline preoperative mammogram before breast surgery. If you are under 40 years, routine mammography screening is not recommended as long as there is no history of breast or ovarian cancer in your immediate family. Your surgeon will take a complete history at your consultation and will make recommendations for breast imaging or other referrals, if necessary. Having breast surgery will not change your personal risk of breast cancer, nor will surgery interfere with cancer screening.
After breast augmentation or breast reconstruction with implants, we teach you how to massage your implants each day so that your breasts remain soft, mobile and natural. The purpose of implant massage is to avoid hardening of scar tissue around the implant (“capsular contracture“), to make sure your breasts remain supple over time, and to ensure that they maintain their beautiful look and feel over time.
Breast Implant Massage consists of moving your implant around in its “pocket” within the breast. You should be able to make your finger and thumb “meet” through the implant when you squeeze your breast (this will make sense to you once you have been instructed on breast implant massage). We recommend ten squeezes a day, for as long as you have the implants. Most women do five squeezes in the morning and five at night; others massage when they are warm and relaxed in the shower, and still others squeeze a couple of times when they use the rest room.
Do not worry about squeezing your breast too hard – you cannot break your breast implant! It takes 50 times the force of a mammogram machine compressing an implant to burst its shell, and no human can create this force!
Massaging your breast implants helps you to “get to know your breasts” and to immediately detect a change, should one develop in the future, even years after your implant procedure. Please call our office immediately if you feel a change in the consistency of your breasts (increased firmness or a change in shape). This could be a sign of early capsular contracture and evaluation by your surgeon is necessary. If capsular contracture is starting, it can often be addressed by early aggressive massage and antibiotics. If an implant becomes hard and no treatment is initiated, a contracture may become permanent and surgery is required to surgically remove scar tissue (if the breast becomes distorted or painful).
You will be instructed on breast implant massage at your weekly visits for the first month or so after surgery, and your breasts will be checked at each of your follow up visits with your surgeon. Implant massage functions to some extent as breast self-examination, which is important for all women, as they should “get to know their breasts”. Implant massage is also important in the long run to enable you to detect any changes in your breasts should they occur in the future.
For all patients who have breast implants (cosmetic or reconstructive), we recommend a Single Dose of prophylactic antibiotics One Hour Prior to any procedure that could potentially provoke bacteria from the nose, the mouth or the “gut” (gastrointestinal tract) to enter the bloodstream and create a potential infection of the breast implant. Examples include teeth cleaning, dental procedures, sinus surgery or colonoscopy. This recommendation is similar to prevention of infection of other implants in the body such as joint replacements or if you have a heart murmur.
Only a single antibiotic dose needs to be taken an hour before your dental/sinus/colon procedure. If you are unsure about whether you need to take preventative antibiotics, please call our office for guidance at 415-570-7352. Antibiotics are NOT necessary for minor procedures involving skin only (mole removal, Botox, fillers, etc) or for manicures or pedicures. You not need to continue antibiotics at all after your dental/sinus/colon procedure; the risk of possible infection is over after the procedure is finished.
Scheduling a good teeth cleaning a few days before having breast implant surgery is usually recommended. It is wise to avoid your next dental procedure for 3 months after implant surgery if possible to decrease any potential risk of bacterial infection.
We will provide you with a prescription for these antibiotics and refills as needed for the future. Most individuals will take Amoxicillin, 500 mg tabs (take 4 tablets at once, 1 hour before the procedure). If you are allergic to Amoxicillin or to Penicillin we then recommend Clindamycin, 150 mg tabs (take 4 tablets at once, 1 hour prior to your procedure).
If you develop redness, warmth, pain or swelling of your breast(s) or fever higher than 101°F (38.5°C), please notify the office immediately at 415-570-7352. These are signs and symptoms of infection and could indicate an infection of your breast implant. We will recommend antibiotics and see you as soon as possible in the office for a full evaluation. Waiting too long to be seen or have treatment if you indeed develop the symptoms above could predispose to development of capsular contracture.
After any procedure that involves the abdominal “core”, there is the potential that you will hesitate to take deep breaths and completely fill your lungs with oxygen due to fear or discomfort. Failure to breathe deeply may interfere with wound healing and can predispose to “atelectasis” (incomplete inflation of the air spaces in the lung that if prolonged, can lead to pneumonia).
After your abdominoplasty or DIEP/SIEA flap breast reconstruction, you will be given an “incentive spirometer” (ICS) deep breathing device by Nurses in the hospital. You will be taught deep breathing exercises, how to use the ICS and how to cough while hugging a pillow. These actions help to fully inflate the lungs and to prevent complications related to poor inspiratory effort. Don’t worry: you cannot “burst” your stitches, nor will forceful coughing create any problem. It is vital that you perform deep breathing and coughing every hour that you are awake when you return home from hospital to keep your lungs healthy and facilitate smooth healing.
Abdominoplasty patients wake up from surgery wearing an “Abdominal Binder”. This is a soft, stretchy compression garment that is worn like a thick belt or a girdle that provides gentle postoperative compression to the area of surgery. It is recommended that you wear your binder for 23 hours/day for the first three weeks after surgery to facilitate the best abdominal contour. It can be removed to shower and eventually at night and during quiet activities.
You will likely feel most comfortable wearing the binder when resuming exercise or activities that utilize the abdominal muscles. The binder can be discontinued after 6 weeks; however, many patients enjoy the extra support and comfort their binder provides for 3 months or longer.
DIEP/SIEA flap patients may not be placed in a binder until after their abdominal drains are removed. This is to encourage the best possible mobility and comfort during their hospital stay and to encourage deep breathing and coughing after a free flap breast reconstruction.
Following a tummy tuck or liposuction of the abdomen, an additional layer of soft foam pad dressing may be added beneath the binder for a flat compression surface. This should be worn against the skin for 2-3 weeks after surgery if instructed by your surgeon to encourage a flat skin contour.
After a tummy tuck or DIEP/SIEA flap, you may be most comfortable sleeping with a few pillows beneath your knees to promote gentle knee flexion, similar to the “beach chair position” you were in during your hospital stay. This position takes pressure off your lower back and eases any perceived tension on your abdominal incision. It is impossible for you to burst your incision after surgery, as it is closed in three distinct and strong anatomic layers. However, you may feel most secure in a slightly flexed position when reclining for a week or two after surgery. You do not need to sleep in a chair or a hospital bed; your own bed with a few extra pillows will be the most comfortable!
Likewise, you may not feel able to completely stand up straight or straighten your abdomen early on after abdominal surgery. However, you do not need to walk in a hunched-over position – this will only create stiffness and back pain! If you have been placed in a garment immediately after surgery, the binder will help to support your back and your incision in the front, enabling you to stand up more straight.
Once you feel ready, you may sleep completely flat and walk with your abdomen fully straight. You may not be able to fully arch your back (in yoga or other exercises) for many months after surgery. Be patient, “listen to your body” and follow its lead when resuming strenuous activities.
You may shower with your drains in place as long as you do not have breast implants with breast drains in place (showering may increase the risk of implant infection). If you are unsure about showering, please check with our office. To prevent the drains from dangling during your shower, hang a ribbon, string or long necklace around your neck and clip the drain bulb to the string to allow them to hang without tension.
After liposuction of the abdomen, you will likely be wearing an abdominal binder with a layer of soft foam for additional flat compression when you awake from surgery. For liposuction of the hips and thighs, a special girdle-like compression garment with a hole that allows going to the bathroom without removing the garment will be applied while you are still asleep. Additional specialized compression garments are designed for other areas of the body: arms (sleeves), chest (torso garment or ACE wrap), or chin (chin strap)
It is important to wear your liposuction compression garment continuously for the first 3-5 days after your liposuction procedure. During this period, your swelling will peak and the garment will keep swelling in check. After your first postoperative visit to the office, your incisions will be checked and you may remove your garment daily for a shower.
You should continue to wear your garment “23 hours a day”, taking it off only to shower until your bruising is gone (approximately 2-3 weeks). You can continue to wear the garment under your normal clothes without any evidence you have had surgery. It is recommended you wear compression for up to 6 weeks after surgery in order to speed resolution of “edema” (post-surgical swelling) and to encourage smooth skin contraction to help reshape your new form.
After any type of facial surgery, it is wise to sleep with an additional 2-3 pillows to elevate your head approximately 30 degrees. This will help to decrease swelling after surgery, promote a more rapid recovery and faster resolution of bruising.
The night after facial surgery, you may place an ice pack wrapped in a soft cloth (frozen peas wrapped in a dish towel works well) against the area of surgery for 20 minutes at a time each hour. Be careful not to apply ice for too long, as the cold helps to numb an already relatively insensate area after surgery, and you could sustain a cold injury if ice packs are left on longer than 20 minutes at one time.
During the first few weeks after surgery, like for any type of Plastic Surgery, it is important to avoid elevating your heart rate and blood pressure by not straining (i.e. having a difficult bowel movement), bending over excessively or lifting more than 5 pounds as these activities may predispose to bleeding. Exercise is not permitted for at least a month up to six weeks after surgery. Your surgeon will advise you when normal activity can safely resume after facial surgery.
After all types of Plastic Surgery but particularly in the face, strict sun avoidance is imperative after surgery to avoid “hyperpigmentation” (possible permanent darkening of the skin and the incisions) and sunburn. Wearing a hypoallergenic sunblock of at least SPF 30 is vital and can be worn from a week postoperatively onward. Visit our section on Medical-Grade Skin Care to learn about the products we carry in our office. Many of the products we carry can be worn directly over the skin soon after surgery and double as a foundation or powder makeup.
Dr. Karen Horton has either authored or reviewed and approved this content.
Give us a call or fill out form below to schedule online.
Monday-Friday: 9am - 5pm
Saturday-Sunday: Closed
Monday:
9 AM to 5 PM
Tuesday:
9 AM to 5 PM
Wednesday:
9 AM to 5 PM
Thursday:
9 AM to 5 PM
Friday:
9 AM to 5 PM
Saturday:
Closed
Sunday:
Closed
Dr. Karen M. Horton
2100 Webster St., Suite 520
San Francisco, CA 94115
Phone: 415.923.3067
We are located in the
Pacific Heights District
in the Pacific Professional Building.
 SHOP SKIN CARE
SHOP SKIN CARE*Please note: Our office is no longer a Participating Provider for insurance. We can provide a financial quote for what anticipated surgical fees will be after your consultation.