Dr. Karen Horton has either authored or reviewed and approved this content.
Free fat grafting, also known as “lipo-filling”, is the latest advancement in breast reconstruction. Fat grafting is commonly used by Plastic Surgeons as a reconstructive tool in secondary breast revision surgery or minor outpatient touch-up procedures after the initial breast reconstruction procedure.
In the last several years, free fat grafting has become commonplace in Plastic Surgery and has rapidly developed into a standard tool in breast reconstruction.
Please note: Our office is no longer a Participating Provider for insurance. We can provide a financial quote for what anticipated surgical fees will be after your consultation.
 Free fat grafting refers to the process of “harvesting” fat cells from a part of the body where they are in excess, using liposuction as a reconstructive tool. The area where fat is harvested from is called the fat graft “donor site”, similar to the concept of a free flap donor site used in breast reconstruction. The most common areas where fat graft is harvested from are the abdomen, thighs and/or buttocks, or wherever a patient stores their stubborn fat.
Free fat grafting refers to the process of “harvesting” fat cells from a part of the body where they are in excess, using liposuction as a reconstructive tool. The area where fat is harvested from is called the fat graft “donor site”, similar to the concept of a free flap donor site used in breast reconstruction. The most common areas where fat graft is harvested from are the abdomen, thighs and/or buttocks, or wherever a patient stores their stubborn fat.
Fat cells are removed using tiny incisions that are generally hidden in natural creases of the body, such the belly button, the groin crease, buttock folds or an existing scar (such as after a DIEP or TUG flap). Using a blunt-ended wand called a cannula – just like for cosmetic liposuction – fat cells are vacuumed out of the body via these tiny incisions. The fat cells are collected in a sterile container in the operating room and then washed and further prepared by gentle washing and straining to next be reinjected into a different part of the body.
The free floating fat cells, after being removed from the body, have lost their blood supply and are free-floating – hence the term “FREE fat grafting”. As opposed to a free flap, which carries its own blood supply via small arteries and veins that are disconnected and then reconnected using Microsurgery, a free fat graft does not have an attached blood supply, and the cells are therefore called a GRAFT (no associated blood supply) as opposed to a FLAP (which comes with a blood supply).
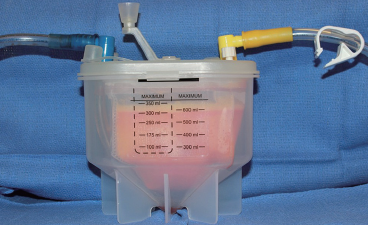
Commercial fat graft collection systems allow fat cells to remain sterile and be gently washed and concentrated before being injected back into the body.
After processing of the fat while the patient is still asleep, the fat cells are injected into a new part of the body – for instance, into a hollow or contour depression at the top of the chest either resulting from a mastectomy or related to a congenital condition such as Poland Syndrome.
When the fat cells are injected into their new location, it is anticipated that some of the fat cells will acquire new blood supply from the surrounding recipient site and remain in that location. However, after fat grafting, regardless of the skill of the surgeon or gentleness of technique, we can only expect around 30% of the fat cells to find a new blood supply and successfully survive in their new location. This is called free fat graft “take”, or fat cell survival.
The process of transplanted fat cells’ survival is very different from what happens with a free flap such as the DIEP flap or the TUG flap in which a segment of structural tissue (skin and fat with all the anatomic connections) carries its own internal circulatory system with it to its recipient site, and where blood vessels are reconnected under the microscope to ensure the flap survives as a whole in its new location.
With a Microsurgical free tissue transplantation (free flap) such as the DIEP flap, SIEA flap or TUG flap, it is expected the fat cells will survive up to 100%, with only very small peripheral areas getting the least blood supply (and resulting in discrete hard areas of firm fat, called “fat necrosis”). This is why a free flap is used for the primary breast reconstruction, and free fat grafting only for small touch-ups afterward. It would be very time consuming and extremely inefficient to attempt to build an entire breast reconstruction using only fat grafting as the primary method!
The future of fat grafting probably involves tissue engineering and 3D printing! I envision that stem cells harvested by liposuction and a three-dimensional construct grown in the laboratory that exactly matches the breast size, shape and dimensions desired by a patient will be possible. It is exciting to imagine how the technology of 3D printing and human biologic tissue engineering can be used to build a breast, and how Microsurgery can then transplant the tissue construct into the body. Exciting possibilities!
Until then, my office offers the latest techniques available for aesthetic reconstruction for women who are facing breast cancer or hereditary increased risk of cancer and are seeking mastectomy.
Since only around 30% of the transplanted fat cells can be expected to “take” in the recipient site, that means up to 70% of the fat cells will, in turn, not survive and be absorbed, to our dismay. The body naturally clears fat cells that don’t survive, just as when normal fat cells reach their lifespan, expire and turn over elsewhere in the body through natural processes – this is called programmed cell death, or “apoptosis”. In order to account for the small amount of fat graft survival, the area is over-filled (if possible) to take into account for partial “take” expected after fat grafting.
There is an external expansion system that some surgeons use for their patients called the BRAVA device. This process involves wearing a contraption on the chest that essentially is two suction cups attached to a machine that sucks the breast tissue into the cups at least 10 hours a day for several weeks to months before fat grafting is performed. The theory is that the suction will increase blood flow to the breasts and potentially improve survival of fat cells with grafting.
Incredibly, some women are willing to commit to this machine in the hopes that the suction will increase circulation to the area, increase the volume of tissue that may accept an implant and improve free fat graft cell survival. Research is ongoing in this area, and most Plastic Surgeons who perform breast reconstruction have not incorporated this device into their practices.
Unfortunately, no. It is necessary for a breast mound to already be present for a patient to wear the BRAVA machine, and by the description, you can imagine that it is not likely comfortable, fun or user-friendly at all to wear! Even if the external suction device was worn religiously for the recommended time, a very thin mastectomy skin flap would not be expected to expand its volume so much that fat graft take would be significantly improved.
The predicament for the slender, thin-skinned breast reconstruction patient where the recipient site cannot accept a significant amount of fat remains the same. It is difficult to inject a great deal of fat into a thin, unhealthy or radiated area.
See a recent blog post on the topic of free fat grafting to the breast to learn even more. The only solution in this situation (very thin chest skin after mastectomy or lumpectomy, radiation, infections or complications, implant rippling or an unsatisfactory breast reconstruction) would be to perform a free flap reconstruction using abdominal tissue or inner thigh tissue, and to bring additional healthy, thicker tissue to the chest area using Microsurgery.
An implant is visible under the skin for one reason – LACK OF PADDING, also known as very thin skin over the implant. This occurs either because a woman is naturally thin in the chest area or because her mastectomy created very thin coverage for the implant. Regardless of whether an implant is under the muscle or not – such as in immediate single-stage breast implant reconstruction I offer to patients – if a woman has extremely little subcutaneous fat, or if the mastectomy surgeon removed so much of the fat in the area of surgery, an implant might be visible through the skin. This is known as breast implant “rippling” or “wrinkling”, and it is a frustrating problem to correct.
Fat grafting to the area can somewhat improve the appearance of rippling in this situation; however, there needs to be sufficient tissue thickness in the area to accept a significant amount fat graft cells. I often describe the situation as “trying to inject a piece of paper with a cup of water” – the thin paper is not very absorbent, and no matter how hard we try, the paper will not accept much, as opposed to conceptualizing injecting a thick sponge full of the same amount of water. We can always attempt a session of free fat grafting in order to improve implant rippling, but the results may not be as dramatic or successful as we might hope for this situation.
In the United States, there are a variety of recently introduced options to help correct breast implant rippling, including new styles of fuller volume breast implants and other mesh-like products that can be added to improve support of the implant in its space. However, with very thin post-mastectomy skin and lack of padding over the implant, even the very best breast reconstruction can still have some rippling – this is a sign that the implant is soft, there is no capsular contracture and the patient is thin overtop of the implant!
Fat graft harvest usually occurs under general anesthesia in the operating room. This is a sterile environment, and it allows surgeons to harvest as much fat as possible without discomfort or any awareness of the procedure. We usually take fat from the area of the body where fat is in abundance and is unwanted, such as the abdomen, flanks, hips or thighs.
The fat grafting donor site area to be harvested is marked prior to surgery, a short general anesthetic is given, small incisions are made as for cosmetic liposuction and tumescent or “wetting” solution is injected to create constriction of blood vessels, avoid bruising/bleeding and to make the area numb after surgery. Fat cells are removed and collected in a sterile fat graft collection device.
While the patient is still asleep, the fat cells are further processed and transferred to small syringes for reinjection into their new location. Handing of the fat is minimal to avoid trauma to the fat cells and encourage the best possible survival. The fat is not centrifuged in order to avoid cell membrane disruption and adipose cell death, but it is gently washed as per the fat grafting collection system manufacturer’s recommendations.

Multiple small syringes are filled with processed fat before reinjecting it into its new location in the chest area.
Fat graft is transferred to small syringes using sterile technique, and then, by way of tiny incisions in the chest area, the fat is directly injected into the area that is to be filled, such as a hollow at the top of a breast reconstruction or around an implant in order to try to improve rippling.
The incisions are closed with dissolving stitches, and a compression garment such as an ACE wrap, an abdominal binder or a Spanx-like lower body garment is placed on the patients before awakening in the operating room. Fat grafting is often done as outpatient surgery, though an overnight stay is also reasonable if the patient is traveling from far away and/or other procedures are being done at the same time.
A patient with sufficient fat to harvest for grafting (sufficient donor site(s)) and who has a recipient site that would likely accept the fat is a candidate for free fat grafting. These individuals are also considered good candidates for liposuction.
Generally, as much as possible! Visit our blog to see an image of how much fat can be removed after liposuction as an example. The process of fat graft harvest is nearly identical for free fat grafting, but the fat is washed and reinjected into the recipient site rather than discarded.

Liposuction canisters filled with fat after a cosmetic liposuction case. The same amount of fat is often removed in free fat graft harvest, which serves as a bonus to the patient!
If there is not enough fat to harvest, or if the area to be filled is much more than the fat which is available, then fat grafting will not likely be recommended. There are very few “contraindications” (reasons why fat grafting would not be recommended) for fat grafting.
See my website page on liposuction to learn more about risks and potential complications of fat graft harvest, which are the same as for cosmetic liposuction. When the fat graft is injected, it must be distributed evenly through the recipient site. If too much fat is injected in one area, it is possible that none of it may survive, and an oil cyst or area of firm fat necrosis (hard, dead fat) may be created.
While we expect at least 30% of the fat cells to survive, it is possible that none of the fat could take up a new blood supply, and it could all go away (although this is rare). Conversely, some patients have a much better survival of fat graft cells, in the range of 50-70% or more. However, these patients usually have a healthy, thick recipient site that readily accepts the fat graft, such as a free flap breast reconstruction or healthy, thick tissue that is not radiated or have many scars.
After a fat grafting procedure, patients usually go home the same day and are seen back in the office within a week. Bruising is expected for at least a few weeks, and exercise can resume within around three weeks, or when discomfort resolves. Sutures dissolve on their own, and the postoperative compression garment can be discontinued when the bruising goes away, or per the patient’s individual comfort. Numbness of the area where fat was harvested from is expected for several weeks – and potentially up to a few months – as the sensory nerves to the skin recover, just like other types of surgery.
Following fat grafting, firm areas of swelling called “edema” can persist for several months after surgery, particularly in dependent areas most affected by gravity. At around three months, we can expect to see the final results of the fat grafting – i.e. how much fat survived in the recipient area and the new contour of the donor site. It can take up to a full year for ALL post-surgical swelling to go down in the donor sites. Numbness in the operated area is temporary, and postoperative discomfort is usually minimal. See our section on cosmetic liposuction recovery for additional information about recovery after free fat graft harvest.
Free fat grafting is usually incorporated into a secondary or “touch-up” procedure after a primary breast reconstruction with a breast implant or a flap. Fat grafting is also becoming routine as a component of revision breast surgery after an initial breast reconstruction procedure following mastectomy. I usually do NOT recommend that a natural breast or one that still has breast tissue present (and that will be undergoing mammograms in the future) have fat grafting performed.
While it IS possible to add fat to a natural breast, I feel very strongly that doing so can hinder breast cancer detection and mammogram screening, and I usually recommend AGAINST it. Read my blog post on fat grafting to a natural breast to learn more and to fully understand this complex and somewhat controversial issue.
Yes, it is possible to graft fat to nearly any area of the body where augmentation is desired. This includes the buttocks, chest, calves, face, under-eye area, lips and even the backs of the hands where age-related changes are often apparent.
Why would anyone want to have fat grafting in these areas? For the same reason that you would consider augmenting the breasts and buttocks, or have dermal filler injected to add volume or conceal thin, aging skin, free fat grafting can be done to other areas.
Keep in mind that the same caveats exist – there must be enough fat to harvest from a donor site in the body, the recipient site must be thick and healthy enough to accept the fat cells and we can only expect around 30% (on average) of the fat cells to survive. Many patients feel it is a lot of work for very little gain, especially if it is a cosmetic procedure. For this reason, injectable dermal fillers are very popular, especially in my office at Horton SPA!
This is an excellent question! Interestingly, we are only born with a certain number of fat cells, and when they are removed using liposuction, these fat cells are gone forever! As long as you maintain a healthy lifestyle and consistent weight, results at the donor site after liposuction or a free fat graft harvest are permanent. Read my educational blog posts about liposuction which go into additional detail about weight changes after liposuction and expected changes with weight gain and weight loss.
However, when we perform free fat grafting, we save those stubborn fat cells that persist despite diet, exercise and our best efforts, and instead of discarding them, we transplant them to a new location where many of them will survive. In the case of fat grafting to fill in a hollow or contour depression resulting after breast cancer surgery, the result in the recipient site after weight gain could be positive and even beneficial!
Weight gain could theoretically improve the contour of the area to which the fat was injected in the chest after free fat grafting for breast reconstruction. Weight loss could, in turn, cause all fat cells to shrink, including the fat that was transplanted to the chest, with a general loss in fat everywhere. In reality, most people do not have extreme swings in their weight, and results tend to be relatively consistent over time.
I CAUTION patients to beware and be careful about having fat injected into their face, particularly if they are young, they have not yet had children and their weight may increase in the future.
Unfortunately, at some of my professional society meetings, entire expert panels are starting to be dedicated to discussing this exact problem – correcting monstrous deformities resulting from careless fat grafting to the face, cheeks, lips and buttocks (you name it and it’s been done), and with weight gain and changes of aging, patients look strange and even deformed!
“Fringe medicine” procedures, such as careless fat grafting to young peoples’ faces, are increasingly being offered by “cosmetic doctors” who are not Plastic Surgeons and are often not Board Certified by the American Board of Plastic Surgery.
Fat grafting to the face is generally not recommended by board certified plastic surgeons. It is very difficult to remove fat from the face or under the delicate skin of the face because large quantities of fat are not normally stored there, and liposuction is not normally done in these locations. DO YOUR HOMEWORK!
If a patient is a candidate for aumentation to the face, I recommend dermal filler injections by an experienced injector such as Emily Sespaniak, NP of Horton SPA. Most dermal fillers are long-lasting (six months up to two years or longer), but can also be reversible by way of injecting an enzyme that will dissolve the product if the results are no longer wanted.
To summarize, free fat grafting is a wonderful adjunct to breast reconstruction after mastectomy for breast cancer or for Poland Syndrome chest wall reconstruction. The results are not magic, but can achieve a subtle improvement in the recipient site. In many cases, the biggest benefit is to the donor site, as we can contour the abdomen, hips, inner and outer thighs thighs or flanks at the same time as improving the results of breast reconstruction.
Dr. Karen Horton has either authored or reviewed and approved this content.
Give us a call or fill out form below to schedule online.
Dr. Karen M. Horton
2100 Webster St UNIT 520
San Francisco, CA 94115
Phone: 415.923.3067
We are located in the Pacific Heights District in the Pacific Professional Building.
Monday-Friday: 9am - 5pm
Saturday-Sunday: Closed
Monday:
9 AM to 5 PM
Tuesday:
9 AM to 5 PM
Wednesday:
9 AM to 5 PM
Thursday:
9 AM to 5 PM
Friday:
9 AM to 5 PM
Saturday:
Closed
Sunday:
Closed
Dr. Karen M. Horton
2100 Webster St UNIT 520
San Francisco, CA 94115
Phone: 415.923.3067
We are located in the
Pacific Heights District
in the Pacific Professional Building.
 SHOP SKIN CARE
SHOP SKIN CARE*Please note: Our office is no longer a Participating Provider for insurance. We can provide a financial quote for what anticipated surgical fees will be after your consultation.